New Delhi: The COVID-19 pandemic resulted in an unprecedented health and humanitarian crisis threatening the food security and nutrition of millions of people around the world. Hundreds of millions of people were already suffering from hunger and malnutrition before the virus hit, concentrated in South Asian countries such as India. There is a deepening nutrition crisis. Malnutrition in all its forms already affects one in three people worldwide and if population growth and climate change increase as predicted, this could rise to one in two. Estimates portend that by 2022, COVID-19-related disruptions could result in at least an additional 9.3 million wasted children and 2.6 million stunted children, 168,000 additional child deaths, 2.1 million maternal anaemia cases, 2.1 million children born to women with a low BMI. Most of this burden will be contributed by Africa and South Asia. All this could result in about US$29.7 billion in future productivity losses due to excess stunting and child mortality, as per an estimate made by researchers from the World Bank, Johns Hopkins Bloomberg School of Public Health, Asian Development Bank, Global Alliance for Improved Nutrition, Micronutrient Forum and International Food Policy Research Institute.
Research confirms that at least six of the top nine risk factors to global health are related to diet. The effects of poor diets and nutrition leave individuals and countries disadvantaged in the long term. For example, child stunting can have life-long effects in terms of suboptimal cognitive development, ill-health, impaired physical growth and reduced earning potential. Malnutrition severely impacts the productivity of many countries and, in the long term, threatens inclusive growth. Across Africa and Asia, the estimated impact of undernutrition on the gross domestic product (GDP) is 11 per cent every year.
Delivering and sustaining the delivery of high-quality diets, even in times of crisis like COVID-19, will result in a healthier and more productive workforce, leading to increased prosperity, reduced hunger and better food security. Go Corona Go songs and jingles reverberated from multiple corners of our country. To mark the nutrition month or Rashtira Poshan Maah, I present to you my interpretation of what this G-O-C-O-R-O-N-A jingle can entail for policy makers and other stakeholders from a public health and nutrition (PHN) lens.
- Go beyond food security – Many reports emerged in the last decade which showed how food systems are failing us. Those who would benefit from consuming more animal source foods, fruits, vegetables and pulses often find them unaffordable. With no effective social protection systems or measures for reaching the poor and vulnerable people, they often resort to harmful coping mechanisms, including eating less nutritious food, reducing meals, taking their children (especially girls) out of school, or selling livestock and other assets. The Food and Agriculture Organization (FAO) of the United Nations notes that when food prices surge, Asia and the Pacific record the largest increases in the number of undernourished people. Governments should aim to at least provide nutrition security by making nutritious diets and food items like fruits and vegetables, pulses etc affordable, accessible and available. Strengthening social protection systems for nutrition is also vital to ensure the continued supply of healthier choices to our vulnerable populations.
- Optimal nutrition needs to be ensured across the life course- Most policy briefs and reports advocate the creation of multiple entry points for concerted action in the health sector throughout the life cycle. This will promote achieving better convergence of nutrition-specific and nutrition-sensitive interventions at the community and household level. Scale-up delivery of quality and coverage of evidence-based programs targeting the most at-risk areas and population groups should also be prioritized to ensure health and nutrition from womb to tomb.
- Capacity building and strengthening – This is required at multiple fronts- whether its frontline workers or medical and allied workforce or researchers and academia etc. Trained staff who can be mobilized to save lives and livelihoods, focusing attention where the risk is most acute are immensely valuable as we witnessed during COVID times too. Increased and trained nutrition capacity (human and material) to improve nutrition/health outcomes is thus of paramount significance to continue essential PHN services. We must continue to invest in research and data to identify incentives/interventions that increase the availability and affordability of nutritious foods while reducing those for unhealthy products.
- Organize awareness building and behaviour change campaigns – All efforts to elevate and accelerate knowledge dissemination, spreading awareness regarding better dietary choices, etc must be reinforced and sustained. Engaging with and using youth leaders as ambassadors to create demand for nutritious foods among children/students, families etc should be undertaken. Continued and strengthened advocacy to support the food and nutrition agenda through the COVID-19 recovery phase will be crucial. Better informed consumer demand for high-quality, diverse, safe diets can be used to stimulate demand for food products linked to sustainable production. The impact of local actions is often faster and properly designed projects can be replicated and spread. Such projects can also become guideposts to improve policies, pointing ways to achieve national poverty reduction and environmental conservation.
- Reform regulatory framework – Strong policies, strategies and programmes – to support children’s right to nutritious diets and essential nutrition services – are very important. Thus revamp, redesign or reframe policies, programs were needed to build in elements of convergence and accountability. Frame nutrition around healthy diets to reduce all forms of malnutrition. For example, school feeding programs like Mid-day meals can be seen as channels to focus on nutrition and diet quality, not solely on feeding and diet quantity. Surveillance to track changes and produce robust disaggregated data are also essential features to help redesign, reform existing PHN interventions.
- One health focus- This point cannot be overemphasized. Every step and action to invest in a sustainable future are urgently needed and must be encouraged by a combination of policy and civil society action. Environment, food security and livelihoods are co-dependent and thus nature and nurture linkages can no longer be ignored. If the land is degraded or prone to natural hazards, less food is produced and significant food shortages can occur. Food secure communities, especially those reliant on the environment for their livelihoods, require healthy and productive ecosystems. Interventions that focus on short-term benefits and neglect consideration of the environment can jeopardize long-term food security and livelihood opportunities. This diminishes societal resilience and undermines recovery opportunities. Implementing food security programs sensitive to environmental and climatic conditions supports sustainability. Also reducing food wastage will go a long way both in ensuring nutrition security and environmental stability.
- Networks, partnerships and governance in and around nutrition should be strengthened and consolidated – It is imperative to make PHN a priority in all development initiatives. To be effective, good governance must be grounded in evidence about what works to improve maternal and child nutrition. It also requires governments and their partners to have the capacity to turn their commitments for nutrition into action. Strategic partnerships across sectors must eb convened and supported with a range of partners to drive action on maternal and child nutrition. The governance of other allied sectors like food, health, water and sanitation, education, environment and social protection systems must also be strengthened to improve nutrition.
- Augment nutrition financing- It is must to prioritise the ‘Leave No One Behind’ agenda in PHN acknowledging the financial and social implications. Capital expenditure needs a significant boost at both the state and central level as it yields a multiplier effect on growth and development too. An analysis done by the Accountability Initiative found that every year, allocations remain lower than requirements in our national budget. They noted a 47 per cent gap in just supplementary nutrition programs alone. In terms of global estimates too, an additional US$1.2 billion per year will be needed to mitigate the COVID effects by scaling up nutrition interventions. Governments and donors must maintain nutrition as a priority, continue to support resilient systems and ensure the efficient use of new and existing resources. All nutrition financing must be transparent and accountable, both domestically, through the timely release of allocations and disbursement, and globally, through the tracking of aid flows and pledges.
Current pessimistic trends do not have to persist if the right actions are taken now and in the coming decades. Better diets are possible. Better health is possible. GO-CORONA should help all stakeholders to capitalize on the pandemic as an opportunity to promote healthy diets and nutrition behaviours to boost the immune system and reduce risk factors for increased severity and poor outcomes from COVID-19. This Nutrition Month should be dedicated to building back better with science, solidarity and evidence-based solutions!
Dr Shweta Khandelwal is Head, Nutrition Research and Additional Professor, Public Health Foundation of India and Program Manager India Taskforce, Lancet COVID commission
Disclaimer: The opinions expressed within this article are the personal opinions of the author. The facts and opinions appearing in the article do not reflect the views of NDTV and NDTV does not assume any responsibility or liability for the same.
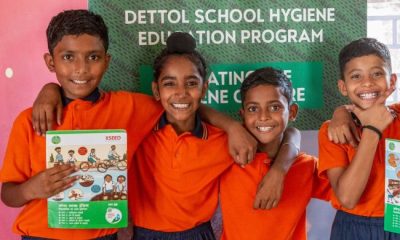
NDTV – Dettol Banega Swasth India campaign is an extension of the five-year-old Banega Swachh India initiative helmed by Campaign Ambassador Amitabh Bachchan. It aims to spread awareness about critical health issues facing the country. In wake of the current COVID-19 pandemic, the need for WASH (Water, Sanitation and Hygiene) is reaffirmed as handwashing is one of the ways to prevent Coronavirus infection and other diseases. The campaign highlights the importance of nutrition and healthcare for women and children to prevent maternal and child mortality, fight malnutrition, stunting, wasting, anaemia and disease prevention through vaccines. Importance of programmes like Public Distribution System (PDS), Mid-day Meal Scheme, POSHAN Abhiyan and the role of Aganwadis and ASHA workers are also covered. Only a Swachh or clean India where toilets are used and open defecation free (ODF) status achieved as part of the Swachh Bharat Abhiyan launched by Prime Minister Narendra Modi in 2014, can eradicate diseases like diahorrea and become a Swasth or healthy India. The campaign will continue to cover issues like air pollution, waste management, plastic ban, manual scavenging and sanitation workers and menstrual hygiene.
[corona_data_new]