Washington: According to research, a mother’s consumption of ultra-processed foods appears to be associated with an increased risk of overweight or obesity in her children, regardless of other lifestyle risk factors. The findings of the study were published in The BMJ. The researchers say further study is needed to confirm these findings and to understand the factors that might be responsible. But they suggest that mothers might benefit from limiting their intake of ultra-processed foods, and that dietary guidelines should be refined and financial and social barriers removed to improve nutrition for women of child bearing age and reduce childhood obesity.
Also Read: The Obesity Challenge And How To Combat It With Diet
According to the World Health Organization, 39 million children were overweight or obese in 2020, leading to increased risks of heart disease, diabetes, cancers, and early death.
Ultra-processed foods, such as packaged baked goods and snacks, fizzy drinks and sugary cereals, are commonly found in modern Western style diets and are associated with weight gain in adults. But it’s unclear whether there’s a link between a mother’s consumption of ultra-processed foods and her offspring’s body weight.
To explore this further, the researchers drew on data for 19,958 children born to 14,553 mothers (45% boys, aged 7-17 years at study enrollment) from the Nurses’ Health Study II (NHS II) and the Growing Up Today Study (GUTS I and II) in the United States.
The NHS II is an ongoing study tracking the health and lifestyles of 116,429 US female registered nurses aged 25-42 in 1989. From 1991, participants reported what they ate and drank, using validated food frequency questionnaires every four years.
The GUTS I study began in 1996 when 16,882 children (aged 8-15 years) of NHS II participants completed an initial health and lifestyle questionnaire and were monitored every year between 1997 and 2001, and every two years thereafter.
Also Read: Health Of Our Environment Interlinked With The Health Of Humans, Especially Mothers: Dia Mirza
In 2004, 10,918 children (aged 7-17 years) of NHS II participants joined the extended GUTS II study and were followed up in 2006, 2008, and 2011, and every two years thereafter.
A range of other potentially influential factors, known to be strongly correlated with childhood obesity, were also taken into account. These included mother’s weight (BMI), physical activity, smoking, living status (with partner or not), and partner’s education, as well as children’s ultra-processed food consumption, physical activity, and sedentary time.
Overall, 2471 (12%) children developed overweight or obesity during an average follow-up period of 4 years.
The results show that a mother’s ultra-processed food consumption was associated with an increased risk of overweight or obesity in her offspring. For example, a 26% higher risk was seen in the group with the highest maternal ultra-processed food consumption (12.1 servings/day) versus the lowest consumption group (3.4 servings/day).
In a separate analysis of 2790 mothers and 2925 children with information on diet from 3 months pre-conception to delivery (peripregnancy), the researchers found that peripregnancy ultra-processed food intake was not significantly associated with an increased risk of offspring overweight or obesity.
This is an observational study, so can’t establish cause and the researchers acknowledge that some of the observed risk may be due to other unmeasured factors, and that self-reported diet and weight measures might be subject to misreporting.
Other important limitations include the fact that some offspring participants were lost to follow-up, which resulted in a few of the analyses being underpowered, particularly those related to peripregnancy intake, and that mothers were predominantly white and from similar social and economic backgrounds, so the results may not apply to other groups.
Nevertheless, the study used data from several large ongoing studies with detailed dietary assessments over a relatively long period, and further analysis produced consistent associations, suggesting that the results are robust.
The researchers suggest no clear mechanism underlying these associations and say the area warrants further investigation.
Nevertheless, these data “support the importance of refining dietary recommendations and the development of programs to improve nutrition for women of reproductive age to promote offspring health,” they conclude.
Also Read: What Causes Obesity, How Can It Be Prevented? Nutritionist Tapasya Mundhra Explains
(This story has not been edited by NDTV staff and is published from a syndicated feed.)
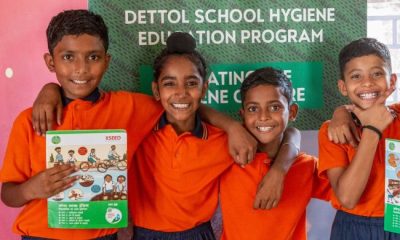
NDTV – Dettol have been working towards a clean and healthy India since 2014 via the Banega Swachh India initiative, which is helmed by Campaign Ambassador Amitabh Bachchan. The campaign aims to highlight the inter-dependency of humans and the environment, and of humans on one another with the focus on One Health, One Planet, One Future – Leaving No One Behind. It stresses on the need to take care of, and consider, everyone’s health in India – especially vulnerable communities – the LGBTQ population, indigenous people, India’s different tribes, ethnic and linguistic minorities, people with disabilities, migrants, geographically remote populations, gender and sexual minorities. In wake of the current COVID-19 pandemic, the need for WASH (Water, Sanitation and Hygiene) is reaffirmed as handwashing is one of the ways to prevent Coronavirus infection and other diseases. The campaign will continue to raise awareness on the same along with focussing on the importance of nutrition and healthcare for women and children, fight malnutrition, mental wellbeing, self care, science and health, adolescent health & gender awareness. Along with the health of people, the campaign has realised the need to also take care of the health of the eco-system. Our environment is fragile due to human activity, which is not only over-exploiting available resources, but also generating immense pollution as a result of using and extracting those resources. The imbalance has also led to immense biodiversity loss that has caused one of the biggest threats to human survival – climate change. It has now been described as a “code red for humanity.” The campaign will continue to cover issues like air pollution, waste management, plastic ban, manual scavenging and sanitation workers and menstrual hygiene. Banega Swasth India will also be taking forward the dream of Swasth Bharat, the campaign feels that only a Swachh or clean India where toilets are used and open defecation free (ODF) status achieved as part of the Swachh Bharat Abhiyan launched by Prime Minister Narendra Modi in 2014, can eradicate diseases like diahorrea and the country can become a Swasth or healthy India.