Highlights
- India has around 10 lakh severely malnourished children: Centre
- Obesity is increasingly becoming a health issue in the country: Expert
- India has fallen behind in alleviating poverty, addressing hunger: Expert
New Delhi: According to the United Nations Children’s Fund (UNICEF), malnutrition is a major contributor to disease burden in India and a predominant risk factor for death among children younger than 5 years of age. It says that well-nourished children become healthier adults as they are able to grow, learn, play and participate better in their communities and are also more resilient in the face of crisis. However, as evident from the government data, many children are unable to get the nutrition they need because of which undernutrition, malnutrition and rising overnutrition are still pressing issues in the country. In March this year, the Ministry of Women and Child Development (MWCD) said that the country has around 10 lakh children with Severe Acute Malnutrition. NDTV spoke to experts to learn about the reasons why the country has been lagging behind on the national and global nutrition-related target even though it has been undertaking various measures to address the issue.
Malnutrition And Anaemia In India: How Big Is The Problem?
The first phase of the National Family Health Survey (NFHS)-5, which was conducted in 17 states and five Union Territories (UTs) in 2019, shows a worsening of performance in all the parameters related to malnutrition. The available data shows an increase in child wasting (low weight for height) in states like Telangana, Kerala, Bihar and Assam, compared to the previous round of the same survey in 2015-16.
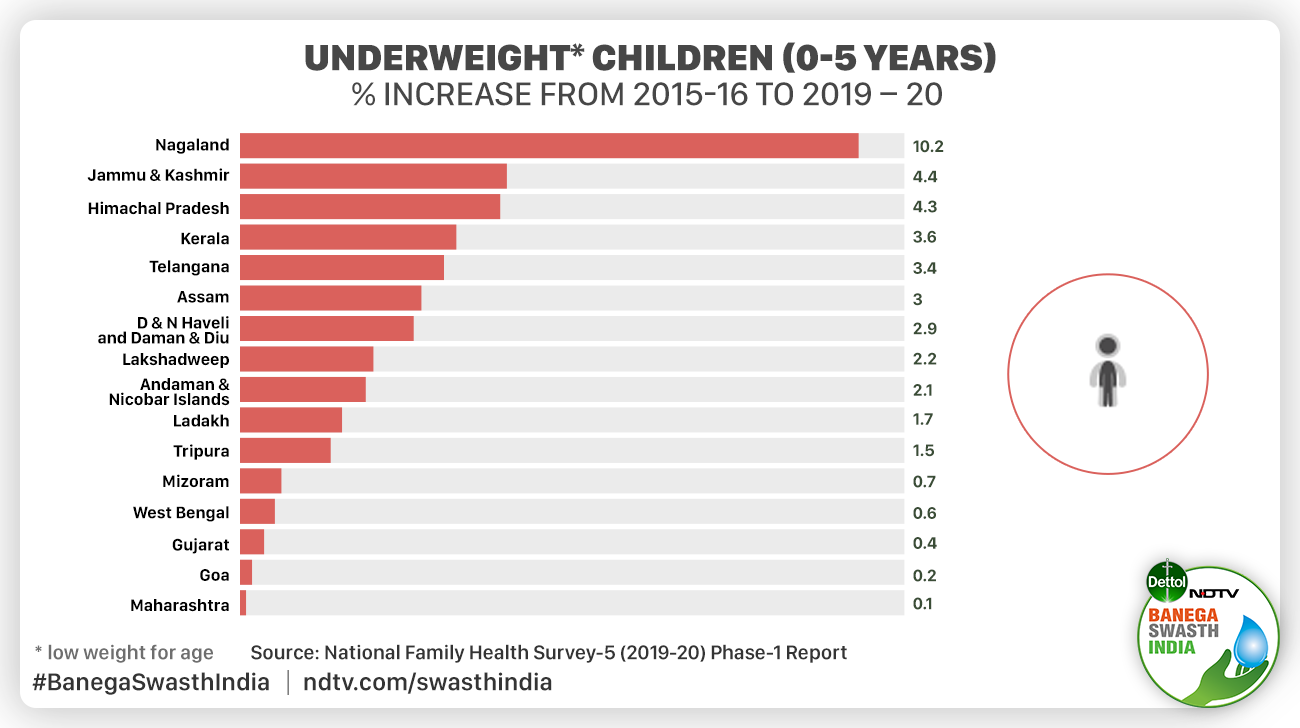
Stunting (low height for age) has increased in states like Telangana, Kerala, Himachal Pradesh and Goa. When it comes to the proportion of underweight children, again, several big states, Gujarat, Maharashtra, West Bengal, Telangana, Assam and Kerala, have seen an increase.
The National Family Health Survey- 4 (NFHS-4) that was done in 2015-16 revealed that in India, 38.4 per cent of children under the age of five were stunted, 35.7 per cent were underweight, 21 per cent are wasted, 18 per cent of children were born with low weight (less than 2.7 kilograms).
According to Dr Dipa Sinha, Assistant Professor, Ambedkar University Delhi, the NFHS-5 data that has been released might not be complete but it does provide some indication regarding the status of malnutrition in the country which is close to the reality. She said,
The NFHS-5’s phase two data was collected after COVID-19 pandemic hit the country. So if anything it would have gotten worse. So, it is not like if the data from other states come, then the nutrition-related indicators would record an improvement. We know from so many sources that Covid and the subsequent lockdowns have had a bad impact on nutrition-related services.
Dr Shweta Khandelwal, Head, Nutrition Research at the Public Health Foundation of India (PHFI), Delhi said that obesity is increasingly becoming a health issue in the country. The share of obese men increased in 19 of the 22 states and Union territories for which the data was available. The share of obese women increased in 16 states. Dr Khandelwal said,
Obesity has been skyrocketing and NFHS-5 preliminary findings have started to confirm this massive rise across all states.

The first phase data of NHFS-5 shows that overweight among children has decreased in only 2 states/UTs
As per the NFHS-5, anaemia, a medical condition in which a person has a lower number of red blood cells, thereby reducing the ability of their blood to carry oxygen to the body’s organs continues to be a worrying condition among children, women and men almost all across the country.
The findings of the first phase of NFHS-5 show that among children, anaemia has increased in 16 out of 17 states and two out of five UTs that were surveyed under NFHS-5. The improvement in the status of anaemia among children was recorded in only Meghalaya and the UTs of Andaman & Nicobar Islands, Dadra & Nagar Haveli and Daman & Diu and Lakshadweep.
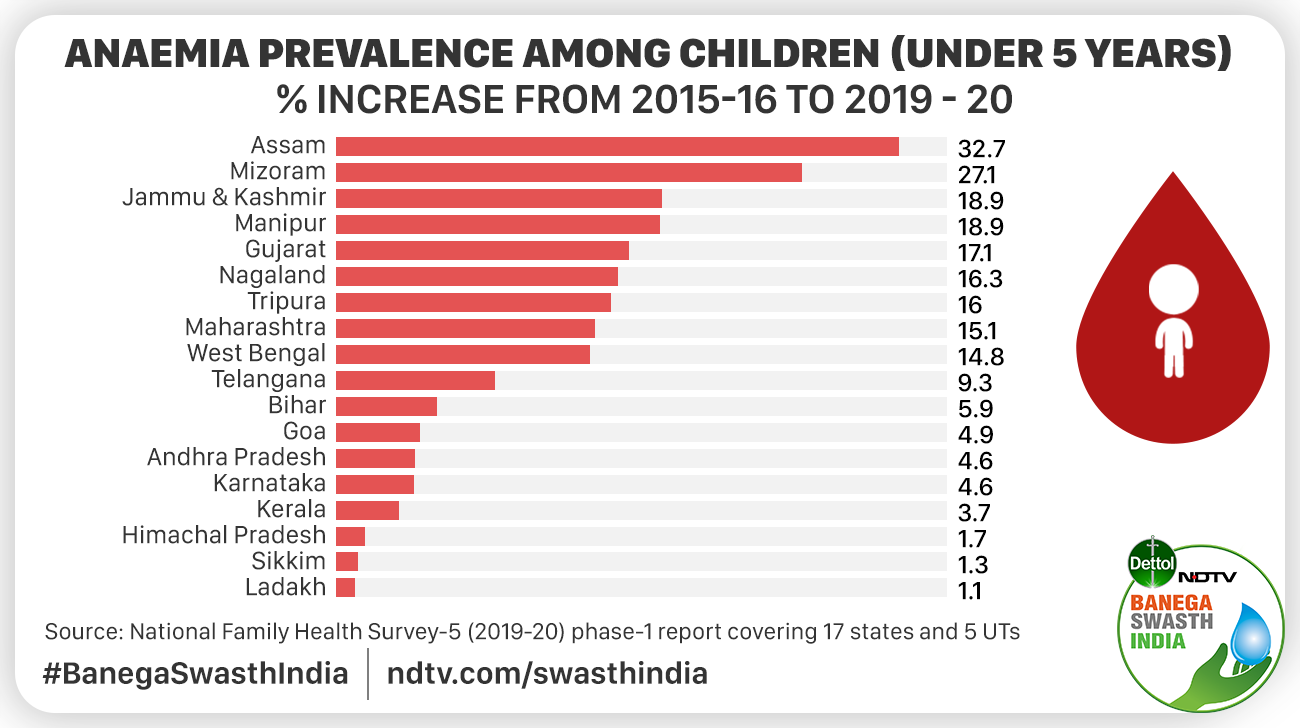
Anaemia prevanalce among children has increased in 18 states/UTs, as per the findings of the first phase of NFHS-V

Anaemia prevanalce among children has decreased in 4 states/UTs, as per the findings of the first phase of NFHS-V
The data shows the prevalence of anaemia among women in the age group 15-49 has increased in 14 states and two UTs. With 71.4 per cent of the total women surveyed suffering from the condition, West Bengal has the highest prevalence of anaemia among women (15-49 years) in the country.
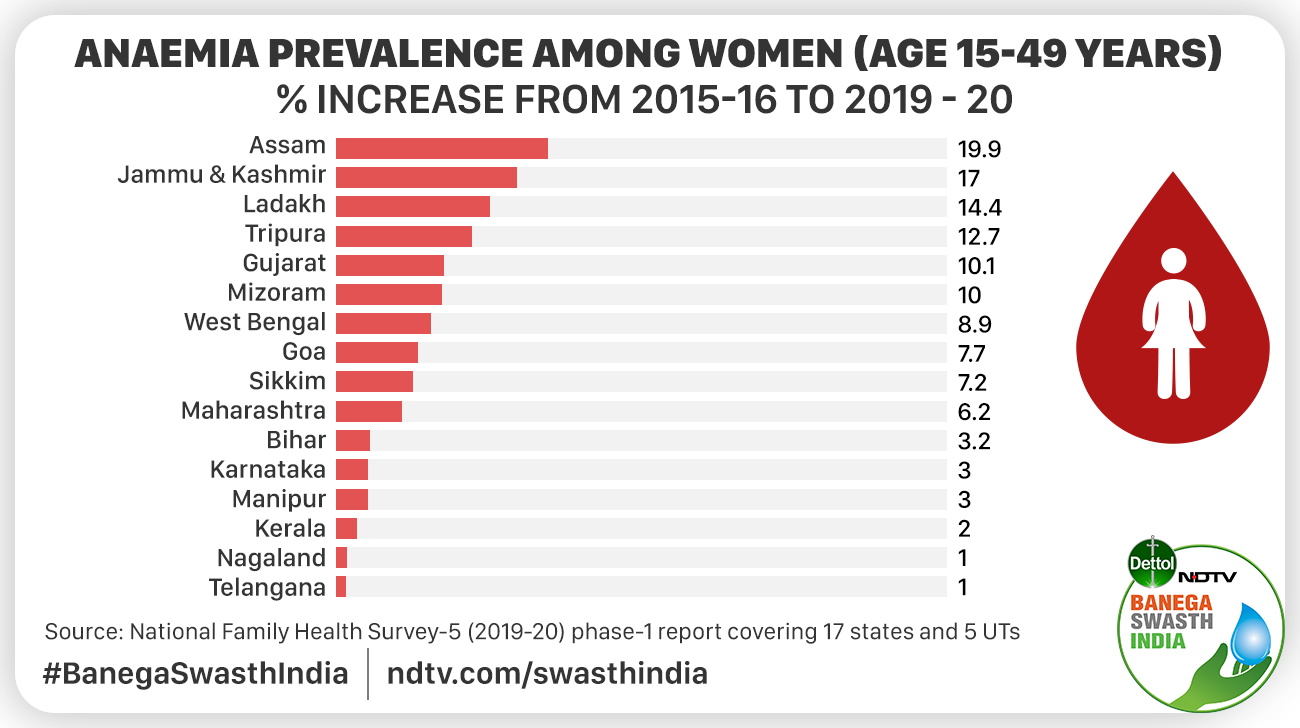
Anaemia prevalence among women has increased in 16 states/UTs, as per the findings of the first phase of NFHS-V

Anaemia prevalence among women has decreased in 6 states/UTs, as per the findings of the first phase of NFHS-V
The data reveals that the prevalence of anaemia among pregnant women has increased in 13 states/UTs. Almost 9 states/UTs have recorded an increase in anaemia among pregnant women.

Anaemia prevalence among pregnant women has increased in 13 states/UTs, as per the findings of the first phase of NFHS-V

Anaemia prevalence among pregnant women has decreased in 9 states/UTs, as per the findings of the first phase of NFHS-V
NFHS-5 has shown that anaemia is worsening across most states and in the majority of our population. This is a serious issue that requires attention and discussion. Anaemia has several consequences like poor cognition, decreased productivity, sub-optimal health among others, said Dr Khandelwal.
Global Targets
The United Nations Sustainable Development Goal (SDG) 2- Zero Hunger aims to end all forms of malnutrition, including stunting and wasting in children under five years of age by 2030 and address the nutritional needs of adolescent girls, pregnant and lactating women, and older persons.

United Nations Sustainable Development Goal (SDG) 2- Zero Hunger aims to end all forms of malnutrition by 2030
According to NITI Aayog, which measures the country’s progress on SDG targets, only Kerala and Chandigarh are performing well on Goal 2. NITI Aayog’s Sustainable Development Goal Index 2020-21 shows that while India as a whole has improved its score from 35 in 2019 to 47 in 2020 out of 100 on Goal 2, the performance is still poor. For becoming a performer, India needs to have a score of 50-64 while to be a frontrunner, it should score over 65.
Commenting on the status of the country on achieving SDGs, Dr Khandelwal said,
NITI Ayog’s Sustainable Development Goals Index 2019-20 showed that India has fallen behind in alleviating poverty resulting in several states and UTs failing to address hunger and malnutrition. All this is pre-COVID data. Come COVID-19 and we are further slipping on almost all public health nutrition targets. Given the acceleration of the pandemic in many low- and middle-income countries, particularly in populous countries in South Asia like India that had high rates of malnutrition pre-COVID, the real impact may be even more devastating than anticipated. In these settings, the consequences may be closer to the most pessimistic scenario, with the possibility of an additional 1.36 crore wasted children, 36 lakh stunted children, and 2.8 lakh child deaths by 2022, as per an estimate. In addition, 48 lakh maternal anaemia and 30 lakh women with low body mass index.
National Targets And Ongoing Efforts To Tackle Malnutrition
The National Nutrition Mission that was launched in 2017 to tackle malnutrition set the target of reducing stunting, underweight, and low birth weight, each by 2 per cent per year; and anaemia among young children, adolescents and women each by 3 per cent per year. It also aimed to strive for reducing stunting to 25 per cent by 2022 along with a 2 per cent reduction every year. The mission was renamed POSHAN (Prime Minister’s Overarching Scheme for Holistic Nutrition) Abhiyaan in March 2018.
This year, the POSHAN Abhiyan has been intensified in the form of Mission POSHAN 2.0 and the ‘Saksham Anganwadi’. Anganwadis under the Integrated Child Development Scheme (ICDS), according to the central government, is the largest nutrition supplementation programmes in the world. It is implemented in two ways: Take Home Ration (THR) of food supplements for 6-36 months-old children and, on-site Hot Cooked Meals (HCM) for pregnant and lactating women and children aged 3-6 years.
Apart from POSHAN and ICDS, the National Food Security Act (NFSA) that covers over 80 crore people has been making efforts to curb hunger and ensure food security for people through the Public Distribution System (PDS) which includes 35 kg of foodgrains per month to households eligible under Antyodaya Anna Yojana (AAY) and 5 kg of foodgrains per person per month to Priority Households (PHH) beneficiaries at a subsidised cost of Rs. 2 per kg of wheat and Rs. 3 per kg of rice. Similarly, the ‘National Programme of Mid-Day Meal in Schools launched in 1995 aims to enhance enrolment, retention, and attendance and simultaneously improving nutritional levels among children.
To fight anaemia among women of reproductive age, India launched the National Nutritional Anemia Prophylaxis Programme as early as 1970, as per the Central Government which focused on distributing the Iron-Folic Acid tablets. The programme was revised and expanded to include beneficiaries from all age groups such as children, adolescents, pregnant and lactating women and women in the reproductive age group under the National Iron Plus Initiative (NIPI) programme in 2011. In December 2019, the Government of India launched the Anemia Mukt Bharat (AMB) under POSHAN to strengthen the fight against anaemia. AMB focuses on organising Test-Treat-Talk (T3) anaemia camp for testing for anaemia, treating with Iron-Folic Acid tablets and talking to people about iron, protein and vitamin C rich foods and healthy lifestyle measures.
The nationwide lockdown in India in 2020 due to the COVID-19 pandemic had a negative impact on the implementation of nutrition and food-related schemes. Dr Sinha said,
During the Covid crisis, initially, when the lockdown started, there was an issue of movement, fear of infection, Anganwadi workers were engaged in raising awareness on COVID-19 and contact tracing. However, soon, in about two months, the services were resumed everywhere. The strategy adopted by the government to handle nutrition schemes and services has been the provision of supplementary food and rations at the doorstep of beneficiaries and Take Home Ration through Anganwadi centres. However, to safeguard pregnant women and manage vulnerable children in rural areas, the government must resume provision of hot-cooked meals.
The reverse migration that occurred during the pandemic-induced lockdown, leading to the displacement of many migrant workers and their families in urban areas due to loss of livelihood, returning to their villages. This meant an increase in the number of mouths to feed in families in rural areas. According to Dr Sinha, the Pradhan Mantri Garib Kalyan Anna Yojana (PMGKAY) of the centre that provided 5 kilograms of free ration and 1 kilogram of pulses to over 80 crore poor people over and above their regular entitlement under the PDS for about a year has proved that public distribution system is the backbone of efforts towards addressing hunger. She stressed making PDS universal which should be initiated by including the poor and the needy without ration cards.
Why Is India Struggling On The Malnutrition Front
According to experts, India is unlikely to meet targets set under the POSHAN Abhiyaan or the Sustainable Development Goals for the reduction in the prevalence of stunting, underweight, low birth weight and anaemia in women and children by 2022 and 2030 respectively. Dr Sinha said,
As the indicators are showing, we are not on target at all. While, the complete data is not released yet, but the NFHS 5 data that we have right now shows that in the five years between 2014-19, there has been no reduction in any form of malnutrition. Even if we don’t say that it has become worse across the country, it has definitely not improved and even the few states that are showing some improvement, the gains are much less than what our targets are. If we look at SDG targets, I would say that it is not possible for India to achieve the Zero Hunger Goal and the target of eradicating stunting, wasting and underweight completely by 2030. Not just in India but everywhere in the world, Covid has taken a toll on food security everywhere.
Discussing reasons behind the holdup in achieving the nutrition targets, Dr Sinha said there are many factors affecting it like poverty, consumption and expenditure along with gaps in the implementation of various schemes and programmes. She said,
There is a lack of adequate data to know the exact reasons for the lag in progressing on nutrition targets. Apart from complete NFHS-5 data, we need data from National Sample Survey (NSS) which provides information on people’s economic status and calorie consumption. We have not got the NSS data after 2011-12. So, we can only say on the basis of what we see on the ground and slowdown in the average economic growth rate IS the major reason.
According to the World Food Programme, COVID has pushed additional 15 crore people worldwide into extreme poverty and the number of people facing food insecurity and hunger are on the rise because of the pandemic, together with persistent conflicts and climate change. Basanta Kumar Kar, International Development Professional, Recipient of the Global Nutrition Leadership and Transform Nutrition Champion Award highlighted that since the COVID-19 pandemic started in the country, crucial government schemes have faced interruptions especially in the underserved regions affecting lakhs of tribal and other marginalised communities.
However, as per experts, the country was struggling with malnutrition even during the years leading up to COVID-19 years. According to Dr Sinha, the period between 2015-2019 was not economically good, especially for the people engaged in the unorganised sector. There was demonetisation that hit the poor badly, implementation of the Goods and Services Tax and inflation that further impacted the poor.
These were shocks that affected the poor more. As a result, we saw that there was a stagnation in rural wages, the inequality increased. It was the time when even Parle G biscuits could not get sold and the company saw huge losses. So, during this period food security did take a hit, Dr Sinha said.
Reduction In Expenditure On Vital Nutrition Schemes:
Another reason for the slow progress under eradicating malnutrition is the reduction in government expenditure on schemes like ICDS, as per Dr Sinha. She said,
If you adjust for inflation, you will see that the expenditure of the government reduced during on important nutrition-related schemes. Poshan Abhiyan is more like a campaign. ICDS- the scheme actually implementing the activities on the ground saw a reduction in the budget. If we look at the period between 2015-2019, a lot of things happened that had an economic impact on people but there has been not an adequate increase in the resources. The Right To Food campaign collated data on starvation deaths in this period and we found over 100 of such cases. Now, after Covid, the situation has worsened.
Union finance minister Nirmala Sitharaman announced her plan to merge schemes under the Umbrella ICDS (Integrated Child Development Services) and the POSHAN Abhiyan to strengthen nutritional content, delivery, outreach and outcome during her Budget 2021-22 speech on February 1, 2021. The new scheme is now called Mission Poshan 2.0 and Saksham Anganwadi.
While the allocation for the new Mission Poshan 2.0 and Saksham Anganwadi is Rs. 20,105 crore, it is almost 18 per cent less than the total budget allocated in 2020-21 of Rs. 24,557 core for four schemes which include – Anganwadi Services (erstwhile core ICDS) which got the allocation of Rs. 20,532 crore, POSHAN Abhiyaan with Rs. 3,700 crore, Scheme for Adolescent Girls with Rs. 250 crore and National Creche Scheme with Rs. 75 crore.
The budget allocated for only POSHAN Abhiyaan for the ongoing financial is Rs. 2,700 crore which is about Rs 100 crore less than the amount allocated for the same last year. The Union Budget also shows that the Revised Budget 2020-21 for POSHAN declined significantly to Rs 600 crore from the original allocation of Rs. 2,800 crore.
While talking about the decline in the budget for POSHAN, Dr Sinha said that it is not clear how the merging of the schemes will improve nutrition. She added,
A large decline in the revised estimates reveal that the government could not succeed in implementing the programmes and schemes completely and thus could not fulfil the allocated expenditure. She added reducing the budget for a subject as important as nutrition that urgently needs an increase in government investment is not a positive sign in terms of achieving the ultimate goal of eradicating malnutrition.
Stagnation In Expansion Of Anganwadi Centres:
According to Dr Sinha, during 2005-2015, there was a significant increase in the number of Anganwadi Centres because of which some improvement was recorded in maternal and child malnutrition. She said,
In 2005, there were only 6 lakh Anganwadi centres which increased to over 14 lakh in 2015. So what we saw was a huge expansion of ICDS in those 10 years. What was needed was the improvement to continue because it was still far from 100 per cent coverage. In fact, there was also a need for next-level expansion that if the number of Anganwadis have increased then the focus should be on improving the quality. But that did not happen.
Lack Of Efforts Towards Nutrition Self-Reliance And Delay In Universalisation Of Public Distribution System:
Mr Kar said that while the country has been providing foodgrains to those in need, it is not enough. He said that first, the PDS should be universalised as still a lot of those in need are out of the food security scheme. Along with this, there is also widespread hidden hunger or the lack of nutrition among people. He added that as most people lack awareness about taking diverse foods in their diet, they take most cereal-based diets and ignore other important foods like fruits and vegetables that are sources of vitamins, minerals and other nutrients.
Lack Of Life-Cycle Approach in addressing Anaemia:
According to Monalisa Padhee, Program Head of Women Wellness Initiative at Barefoot College, a non-governmental organisation based in Tilonia, Rajasthan, the issue of anaemia in India is not being addressed from the life-cycle approach which says that women of all ages should be covered under the interventions. This is because anaemia affects women and girls of all ages. She said,
Anaemia is not a condition that has a sudden impact on someone’s body. It affects them gradually but continuously. Young children and pregnant women are the most vulnerable as it affects the cognitive development of children and can cause mortality among severe cases and anaemia in pregnant women put them at risk of pre-term births and of having low-birthweight infants. Therefore, focusing on the first 1,000 days is important. However, putting all efforts to deal with anaemia during 1,000 days only will not solve the problem. We have a high incidence of anaemia because we do not have interventions that address anaemia in women and girls of all ages.
Dr Khandelwal highlighted that ignoring the fact that anaemia is not an iron deficiency issue alone and that just focussing on iron-fortified foods will not help is becoming a roadblock in the fight against anaemia. She said,
Several nutrients are important here while the authorities are only focusing on iron-fortified foods. Our sole obsession (in programs and policy) with feeding or enhancing elemental iron to tackle anaemia in a country as disperse and diverse as India, is short-sightedness. Research shows that improving Vitamin C, B12 and folate intake among other key nutrients may be promising in improving nutritional anaemia. Of course, other nutrition-sensitive interventions like better WASH (water, sanitation and hygiene), mother’s education among others also influence both prevalence and incidence of anaemia.
Way Forward
According to experts, there is a need to reform systems, policies and behaviour to perform optimally in the interest of public health and nutrition.
Increased investment in children:
All the experts that NDTV spoke to stressed that there is a need to increase investment in children. Dr Sinha said,
There has to be an increased focus on children, focus on women, maternity entitlements, sanitation improvement, mid-day meals, daycare facilities all the same things need to be done properly. Malnutrition cannot be addressed by doing just one thing. Multiple things are required to be done.
Nutrition Security – Going beyond food security:
There is a need to go beyond food security by considering the nutritional value of food to improve an individual’s nutritional status, according to Mr Kar.
Nutrition security is about people’s access to essential nutrients and not just calories, he said.
According to Dr Khandelwal, all stakeholders have to work selflessly towards a shared vision in their own capacities to make it possible for masses to achieve zero hunger. She added that policy reforms to strengthen, diversify and improve the PDS, enable the One Nation, One Ration card scheme universally, improve infrastructure and technology to reduce post-harvesting losses, transport and storage losses, are also critical.
Transforming Food Systems:
According to Dr Sinha, because of the increasingly degrading soil quality, due to reasons like pollution, erratic farming, the farm produce is losing nutrients that it was generally rich in. She also emphasised that local nutrition is being impacted because of the focus on economic gains. She said,
Earlier where people used to produce groundnut there they are now producing soya because of the export market, then, of course, it will affect the local nutrition also.
She said that there is a need to make people aware about the need to have locally produced foods as those are richer in nutrients. This can be done through awareness-building campaigns, encouraging farmers to produce more local food by making farming economical for them and by encouraging people to adopt kitchen gardens, she said.
Income growth:
According to Dr Sinha, there are systematic correlations between household income and food and nutrition security. She said that there has to be an increase in the per capita income in the country so that people can have the capability to spend on more nutrient-rich food.
Convergence of the ministries and departments:
Experts said that addressing the issue of malnutrition cannot be done by undertaking just one or two kinds of efforts. It requires the convergence of various ministries and departments like women and child development, education, social justice, health, environment, agriculture, jal shakti, need to work together, they said.
Also Read: Opinion: Fighting Hidden Hunger, Deficiency In Micronutrients With Food Fortification
NDTV – Dettol Banega Swasth India campaign is an extension of the five-year-old Banega Swachh India initiative helmed by Campaign Ambassador Amitabh Bachchan. It aims to spread awareness about critical health issues facing the country. In wake of the current COVID-19 pandemic, the need for WASH (Water, Sanitation and Hygiene) is reaffirmed as handwashing is one of the ways to prevent Coronavirus infection and other diseases. The campaign highlights the importance of nutrition and healthcare for women and children to prevent maternal and child mortality, fight malnutrition, stunting, wasting, anaemia and disease prevention through vaccines. Importance of programmes like Public Distribution System (PDS), Mid-day Meal Scheme, POSHAN Abhiyan and the role of Aganwadis and ASHA workers are also covered. Only a Swachh or clean India where toilets are used and open defecation free (ODF) status achieved as part of the Swachh Bharat Abhiyan launched by Prime Minister Narendra Modi in 2014, can eradicate diseases like diahorrea and become a Swasth or healthy India. The campaign will continue to cover issues like air pollution, waste management, plastic ban, manual scavenging and sanitation workers and menstrual hygiene.
[corona_data_new]